In the October 2020 Brain Health Registry newsletter, we explored some ways the Covid-19 pandemic has disrupted and transformed dementia research. Many research studies have been suspended, while others have migrated online and continued on. Some clinical trials have even moved into peoples’ homes.
As the global community grapples with the pandemic, scientists are striving to learn how the coronavirus can impact the brain and cognition.
And, as the pandemic stretches into 2021, society as a whole continues to reckon with its ramifications for people with dementia, their loved ones, and their caregivers.
Covid’s impact on the brain
Some people who have contracted Covid-19 have experienced concerning neurological symptoms, ranging from loss of taste and smell, to delirium, to stroke. On occasion, symptoms have persisted long after recovery from the virus.
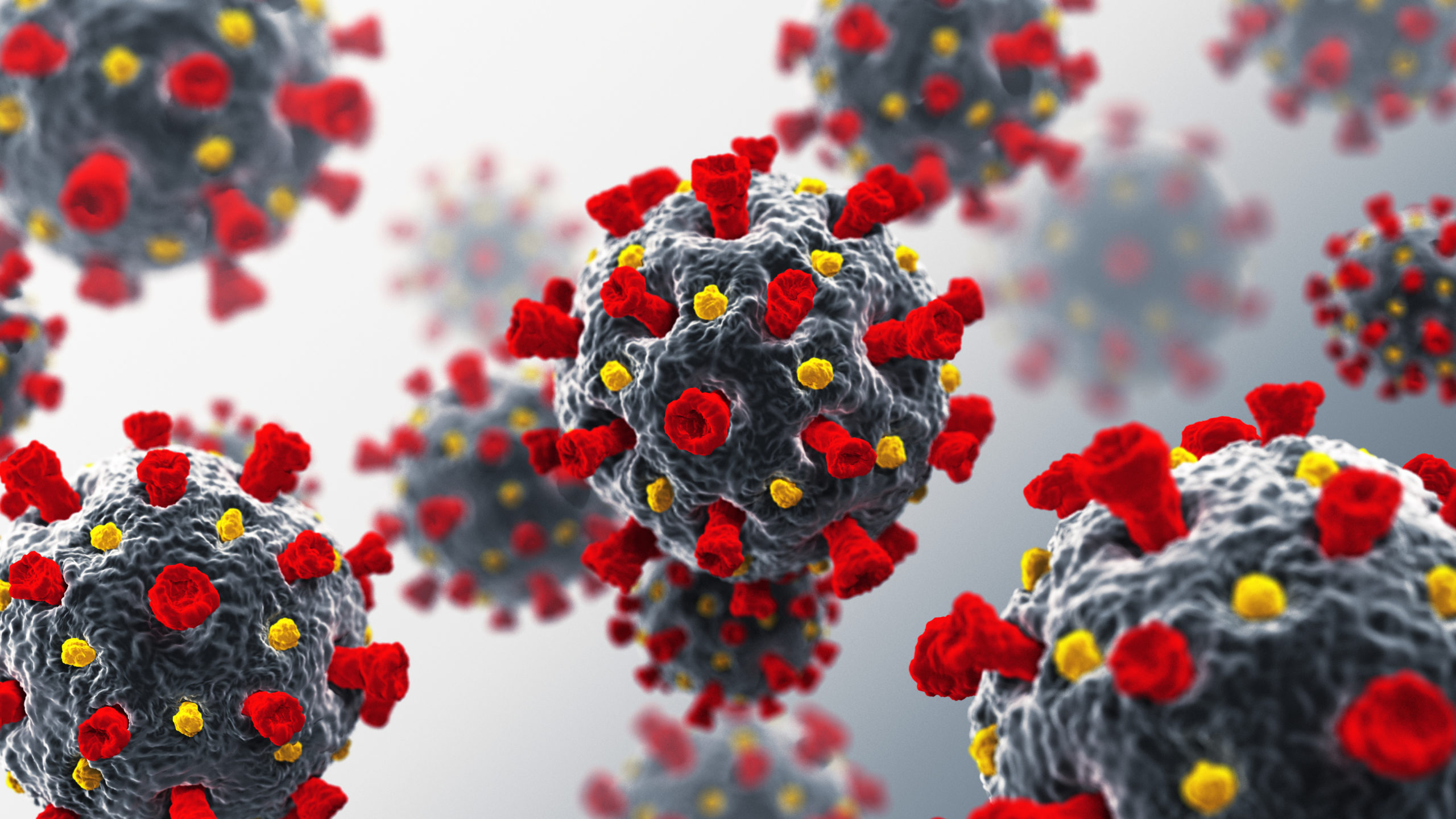
In December 2020, researchers found that the distinctive spike proteins studding the surface of the coronavirus can pass into the brains of mice, triggering an inflammatory response.
Whether the virus can enter human brain cells remains uncertain. A brain donation study from Columbia University did not find the virus directly within post-mortem brain cells, but found extensive damage wrought by the virus. Some researchers think Covid-19 may harm the brain by entering nerve endings or the bloodstream, or by eliciting a powerful immune response that causes inflammation and damage to tissues and organs. Ultimately, we’re still not entirely sure.
Covid and dementia
A study of almost 62 million electronic medical records found that persons with dementia have a higher risk of getting Covid-19, and are also more likely to have severe or fatal cases of the disease. The study also emphasized that the virus is not hitting all communities equally, adding to what is already known about health disparities. The researchers found that Black people with dementia were almost three times as likely as white people with dementia to become infected with the virus.
The pandemic has posed distinct challenges to many individuals living with dementia. Isolation and loneliness have been, and remain, major obstacles. For some, networks of care and daily routines have collapsed.

Researchers in the UK found that during the Covid-19 lockdown, loneliness and decreased physical activity were associated with increased depressive symptoms in adults fifty and older.
Furthermore, being cut off from socialization and visitation likely accelerated cognitive and functional decline in some individuals with Alzheimer’s and related conditions.
Fortunately, as vaccines become more widely available across the United States, families are increasingly able to reunite safely.
—
Know that if you or your loved ones are struggling during this difficult time, you are not alone!
The Alzheimer’s Association has a list of resources for both in-home caregivers, and caregivers in residential facilities.
Other tips for caregivers and individuals with dementia include cultivating a mindfulness or meditation practice, frequent exercise, and getting a good amount of sleep every night. See a list of tips assembled by the UCSF Memory and Aging Center here.